At the spinal column are the elongated columns of bones, which the thoracic ribs support. The thoracic ribs push the bones the length of bone structure.
The ribs join with the spinal column in various areas. Joints connect with these ribs, which are a field of study, since they often wear and tear, causing gradual degenerative diseases, such as osteoarthritis.
Osteoarthritis is defined in medical terms as a metabolically dysfunction of the bones.
The results of the drops in our life-sustaining chemicals, which promote activity causes the bones to reduce mass whilst increasing porosity. The disease can cause osteoporosis to set in and intensify risks of fractures.
How do doctors consider osteoarthritis and/or osteoporosis?
Doctors often consider etiology aspects, including hyperthyroidism, deficiency of estrogen, Cushing’s syndrome, immobility, increases in phosphorus, liver illness, lack of exercise, deficiency of calcium and protein, deficiency of Vitamin D, and bone marrow conditions. Wear and tear of specific joints as mentioned above is also linked to osteoarthritis.
According to Pathophysiology in medical terms, osteoarthritis is assessed by considering the rates of bone resorption that exceeds the rate of the bone structure or formation.
Experts will often test the patient while considering rises in “bone resorption” and increases in phosphate (Salt of Phosphoric Acids) that stimulates the parathyroid activities.
Phosphoric acids will form ester, which emerge from reactions via alcohol, metal, and radicals. If estrogen shows a decrease in resorption, it could also show traits of osteoarthritis.
What are the symptoms?
The symptoms may emerge from Kyphosis or otherwise known as Dowager’s hump.
Back pain, as well as damage to the thoracic and lumbar may be present. In addition, the patient may lose height, and demonstrate an unsteady walk. Joint pain and weakness is also present.
How do doctors determine if osteoarthritis is present?
First, they assess the symptoms and then request tests, such as x-rays and photon absorptiometry.
X-rays of course helps the doctor to locate thinning of bone structures, porous structures in the bones, and rises in vertebral curvatures. The photon tests help the expert to spot decreases in minerals.
What if I test positive for osteoarthritis:
If you test positive then the doctor considers treatment. The treatment often includes management, interventions, and further assessments.
Further assessments help the doctor weed down potential complications. The complications often include pathologic fractures, which are complex.
How does the doctor manage osteoarthritis?
No two people are alike therefore medical management varies. Yet, most doctors set up a high-calcium, protein diet, as well as increasing minerals, vitamin regimens, and boron.
Doctors may include in the management scheme alcohol and caffeine restrictions. In addition, the scheme may compose tolerated exercise, monitoring, lab studies, specifically studies on phosphorus and calcium.
Doctors may also include into your management scheme estrace increase, i.e. estradiol or estrogen intake.
Supplements with calcium carbonates (Os-CAL) are often prescribed as well. Additional treatment includes mineral and vitamin regimens, exercise, and so on.
Many doctors prescribe Aldactazide, Dyazide, which is a thiazide diuretic hydrochlorothiazide. Over-the-counter meds, such as the NAID-based painkillers are prescribed as well.
Prescriptions often include ibuprofen, Motrin, Indocin, Clinoril, Feldene, Ansaid, or flurbiprofen, voltaren, naproxen, Dolobid, and naprosyn is often prescribed.
How intervention helps:
Interventions assisted by nursing staff include balanced diets, pain and musculoskeletal assessment, monitoring, meds, home care instructions, posture training, body mechanic support and training, and so on.
The patient should also be informed about osteoarthritis as outlined by the
Foundation of Osteoarthritis. In addition, the doctor is advised to allow the patient to express his/her emotions, feelings, etc in relation to the illness.
Ways to Relief Common Back Pain
Back pain is blamed, generally for poor muscle tone especially on the affected area. Overall, 90% of chronic back pain sufferers are individuals (professionals, housewives, students…) that seldom see an exercise regimen. And the other 10% have the condition due to injury such as ripped muscles.
If you have back pain, you are not alone. Back pain is one of the most common neurological complaints that physicians diagnose in the United States, next to headache.
So it’s no cause to fret if you have one. And no, most back pain is not always associated with age (though age DOES have an effect on back pain), instead it is the lack of physical activity and deficiency in liquid intake.
Defining the pain is important in order to control it. And for purposes of our definition, we categorize back pain into three categories. We have the Acute Back Pain, Chronic Back Pain, and the Neuropathic Back Pain. Acute back pain is a common type of pain that is directly related to a damage tissue.
It is experienced immediately, characterized by sharp, biting pain of a damaged tissue. It is generally accepted that acute back pain lasts less than 3 months if left untreated.
If the pain persists longer after it has been healed or treated then it falls now under the classification of chronic back pain. Chronic back pain falls into two sub categories: pain with an identifiable pain generator and pain without an identifiable pain generator.
The former obviously has a cause, such as: degenerative disc disease, spinal stenosis, spondylolisthesis and other spinal structure problems due to injury. The latter is more a disease rather than a symptom of an injury. And for purposes
As long as you have no serious physical injury or occurring illness, chronic back pain relief is very achievable. It’s all in the problem approach. First thing is identifying the problem.
Was it just stress or a serious defunct? Don’t be hasty in dismissing it as stress. Look for other telltale signs. Are you having a fever? Are other parts of your body hurting? If so, then look for other signs. Common culprits are appendicitis, hepatitis and gastrointestinal complications.
Next is identifying the pain type. Is it muscular or structural? Structural poses a difficult situation, you may have herniated discs. If muscular, ripped muscle is common but usually harmless.
Doing Tai Chi is one effective chronic back pain relief. It promotes good posture and meditation improves your ability to withstand the pain.
If done regularly, these exercises would equate doing a good aerobic exercise with also eases bad backs.
Bending exercises also helps in chronic back pain relief though somewhat lesser in efficiency.Alternately, you could purchase a back pain machine.
The TENS machine is surprisingly an effective chronic back pain relief and it is handy, portable, and quite cheap.
In a word, I would suggest using a TENS machine for immediate chronic back pain relief and Tai Chi for the long lasting prevention for back pain.
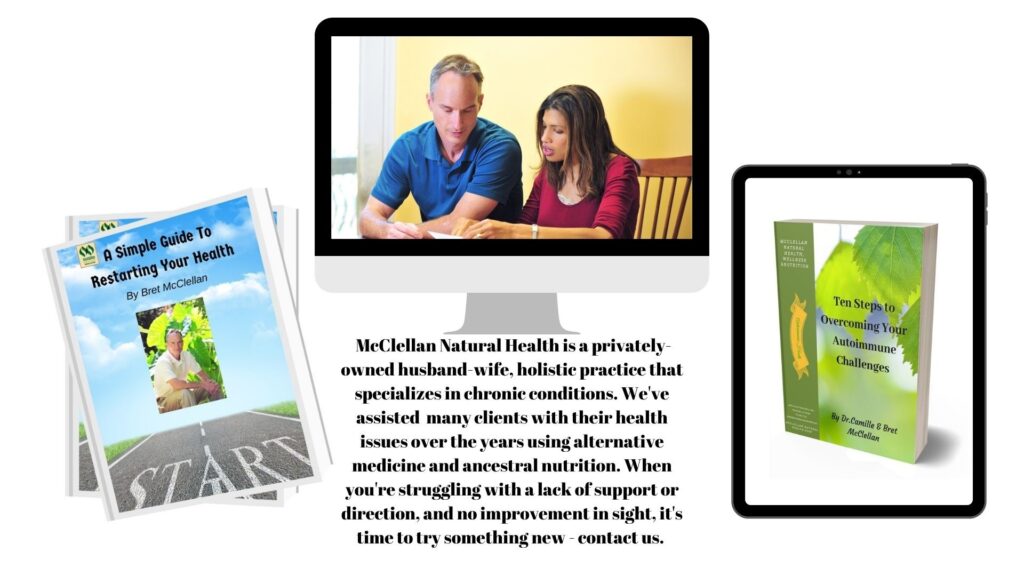
Camille McClellan, MD, DNM, MBS
Naturopathic practitioner
McClellan Natural Health, Wellness & Nutrition
Free Naturopathic/Homeopathic Consults Available